Healthcare Fraud Waste and Abuse AI
Healthcare fraud, waste, and abuse AI is the use of AI to detect bad actors collecting for services that are either non-existent or exaggerated.
Rough estimates suggest that ~30% of US healthcare spending falls under the category of fraud waste and abuse [1]. With 18% of US GDP falling under healthcare, that means that roughly 5% of the US GDP is associated with medical fraud waste and abuse.
How Can We Use Fraud Waste and Abuse AI?
The following can be studied with Artificial Intelligence, as we will discuss:
Fraud and abuse: Exploitation of the healthcare system for financial gain, such as requesting reimbursement from the government for care (Medicare or Medicaid usually) that has never occurred.
Failure of care delivery: Incorrect or delayed care.
Low value care: Ineffective or low-impact care.
The following typically require resolution via Administrative Policy. They may be detectable with AI by analyzing final costs paired with diagnosis.
Administrative complexity: Unnecessary overhead costs associated administrative tasks.
Pricing failure: The price of a treatment is far greater than its cost.
Failure of care coordination: Poor communication or transition of care between facilities.
Fraud Waste and Abuse Data Sources
See our blog on medical data sources. Primarily, medical records (electronic or not), claims, and billing information offer the best data outside of a hospitals doors for the research of fraud waste and abuse. NLP coupled with unstructured healthcare data, or straight up data extraction from HL7 ADT, HL7 CDA, or HL7 FHIR all are firm data sources for this.
While external data sources may provide further information, its important to note that AI systems typically prefer a consistent input when making decisions, so relying on high quality and consistently structured information is far better than relying on data from numerous sources.
Anomaly Detectors in Fraud Waste and Abuse
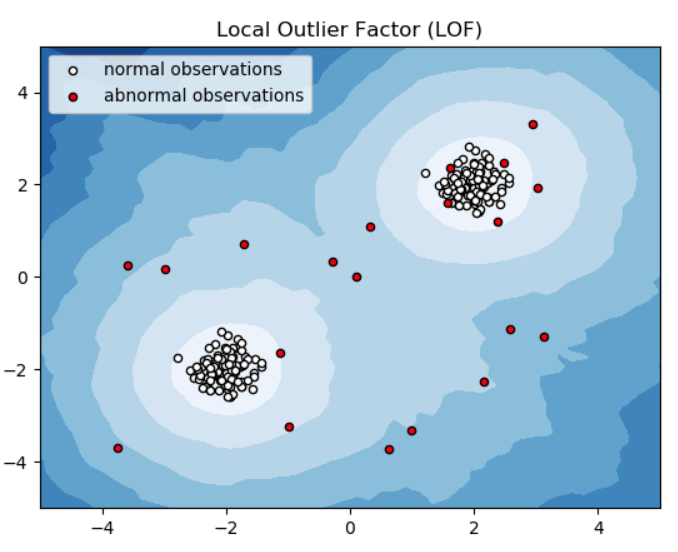
A core technology used with detecting fraud, also used in the credit fraud space are anomaly detectors. There are a core AI technology that ultimately aim to detect data points that are uncommon. Anomaly detectors may be made from traditional machine learning, common neural network architectures, or even LLM networks.
“Uncommon“ of course needs to be defined. Anomaly detectors are not so different than most AI models that seek to give each data point a score between 0 and 1.
One primary difference is that an anomaly detector also requires a threshold where a user draws a line in the sand to say what is and is not likely an anomaly. However, they are also frequently capable of ranking how anomalous each of these datapoints is so they can also be prioritized for human review.
Modern anomaly detectors are not only capable of picking out what the anomalies, but also can point a user to the evidence that flagged it. This is particularly useful for handing to a human for validation and further investigation into the fraudulent action being considered.
Graph Networks in Fraud Waste and Abuse
Graph network databases, as depicted below are a unique type of database that store information on relations between entities and entity information. Easy examples of this are Facebook and Linkedin.
Graph network databases can describe a patient and related info
This tool is also hugely useful for analyzing patients and practitioners, as well as their interactions. Nodes are often patients, practitioner, and or facilities. Edges (also called links) are often interactions between those entities.
Visually this can be helpful, but they also permit queries to better understand relationships. For example if, a practitioner is overprescribing opioids to patients, an anomaly detector plus a graph network will easily be capable of detecting this.
Let’s explore how Tenasol makes use of these technologies in the 3 categories previously mentioned:
1 - Fraud and Abuse AI Detection
The HHS OIG maintains a most-wanted fugitive list of people who have collected government money for care that was never performed. These people typically either charge the government for services not rendered (research or care), or creating equipment/tests/treatments that are bogus.
The following are approaches we employ for detection of these:
Anomaly detectors evaluating claims patterns and medical record patterns of individual practitioners based on their specialty relative to other practitioners with the same specialty.
Graph network analysis of practitioners who may be bad actors who form “islands“ and do not interact enough with other parts of the healthcare ecosystem.
Practitioner anomaly detectors seeking practitioners who frequently diagnose conditions uncommon with their patient cohort.
Anomaly detection of equipment/tests/treatments and their outcomes based on brand identifier.
2 - Failure of Care Delivery AI Detection
As previously mentioned, failure of care delivery happens when there is a patient who is treated incorrectly, or with delayed care. Structured data is highly valuable for this as it permits logical linking of diagnosis with treatment, and accountability to linked practitioners. Specifically, this enables:
Detection of cases where no treatment is documented or
Timing anomaly detector analysis between diagnosis to treatment, based on drug-treatment pairings.
3 - Low Value Care AI Detection
Low value care detection is the detection ineffective treatment. This is performed with an anomaly detector by:
Using a graph network coupled with anomaly detectors to detect high rates of treatments that are inconsistent with diagnosis, such as overprescribing of opioids.
Using an anomaly detector coupled to seek conditions-treatment pairs that are uncommon. This is especially easy to do with HL7 CDA data or HL7 FHIR data.
Conclusion
Detecting fraud, waste, and abuse (FWA) in healthcare using AI is not just an efficiency improvement—it's a necessity for protecting resources and ensuring patient care integrity. AI-powered anomaly detection and graph networks provide powerful tools to identify unusual patterns, whether it’s fraudulent billing, delayed care, or ineffective treatments. By leveraging structured data sources like HL7 FHIR and CDA, AI can detect inconsistencies at scale, allowing for real-time insights and proactive intervention. However, technology alone isn’t enough.
Effective FWA detection requires a combination of AI-driven insights, administrative policy changes, and continuous monitoring. As AI continues to evolve, integrating high-quality, consistent data will be crucial for refining detection models and reducing false positives. By addressing fraud, waste, and abuse with AI, healthcare systems can allocate resources more effectively, reduce unnecessary costs, and ultimately improve patient outcomes. Tenasol remains committed to advancing these AI techniques to drive meaningful change in the industry.